
Dr. Thomas Varghese, a distinguished Surgical Oncologist and Reconstructive Surgeon, brings a wealth of expertise to the field of oncology. With qualifications including MS, FICS (Oncology), FACS, and recognized as an MCh teacher by the Medical Council of India, Dr. Thomas Varghese currently serves as the Medical Director and Head of the Cancer Division at St. Joseph’s Cancer Hospital and Research Centre in Kochi. Dr. Thomas Varghese is deeply committed to advancing cancer treatment and patient care, contributing significantly to the medical community and providing hope to numerous patients.
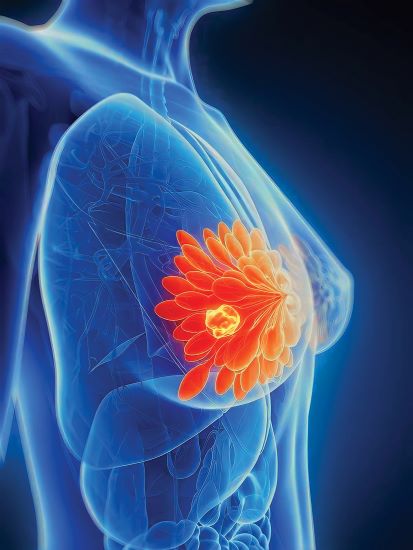
In his insightful article, Dr. Thomas Varghese addresses the challenges posed by breast cancer, emphasizing the psychological impact and societal misconceptions that often accompany a diagnosis.

“Diagnosis of breast cancer can fall like a bombshell into the life of one out of five women in their lifetime” is the tagline that WHO is spreading across continents. Definitely, there is an increase in incidence in the Western world but changes in lifestyles, incorporation of Western lifestyles in own life have changed the scenario in the Third World too. This is shown as an increase in breast cancer incidence even in younger women.
The breast cancer issue is compounded by several factors. Since less than 30 years is no more rarity in cancer incidence, poverty, lack of insurance coverage, and presentation in the locally advanced or metastatic stage are all not uncommon, and many times non-oncologists, treat cancer patients with bizarre end results.
Diagnostic accuracies, and treatment nuances, especially surgical, medical and immune-oncology have progressed in leaps and bounds, however, it’s sad to observe that the percentage of individuals presenting in the advanced stage has not dwindled and remains to the tune of over 50% and death rates also approx 50%.
Apart from the factors mentioned what else could be the driving force for such late presentations?
When we ask breast cancer victims this question, 99% of women in the current generation will have only one answer, “fear of losing breasts”. The wrong information that has percolated in the minds of ordinary women, and even educated lot is in every breast cancer there is a need to “chop breasts” for cure. This fear is circulated far and wide hence many women even refrain from undergoing a screening program, unlike their Western counterparts, to detect cancer in the early stage. But once the cancer diagnosis is disclosed, they are the ones who become hysterical. On several occasions, non-oncologists, and quacks utilize this soft corner and offer unscientific treatments to further push the patients to a non-treatable stage.
Well-educated ladies also will follow this suit and finally perish from a curable status. Since long time in dedicated cancer centers or units, surgical management of breast cancer in the operable stage has been handled by cancer surgeons and later from mastectomy, the concept of BCT, Breast Conservation Therapy evolved.
Cosmetic issues regarding the same forced clinicians to think of better options in the local management of breast cancer and thus “Oncoplastic” procedures evolved. Onco means Cancer, and plasty means to mould.
Breasts are considered as a separate organ in itself, an organ of beauty sign of sexual attraction, bilateral symmetry, and an organ providing confidence to a lady in addition to the primary function of lactation.
Hence such a procedure should offer bilateral symmetry, confidence, sexual attraction, and overall better adjustments with society, workplace, and career.

Oncoplasty urges the cancer surgeon that primary priority is on cancer and the surgical procedure should be oncologically acceptable which can help in avoiding local disease recurrence. There cannot be any corner cutting which is the pre-requisite. The resections are also planned based on the primary evaluation of breast volume tumor volume ratio by an expert, dedicated, breast ultra sonologist and based on the tumor aggressiveness as per core biopsy. We plan reconstructions only when the Frozen section report by the pathologist tells that all the margins of resections are free of disease.
The beauty of this procedure is reconstruction is planned as per resection which may differ from original pre-operative planning.
Although in dedicated centres this procedure has become the norm, the majority of the patients who are evaluated by non-oncology specialists, like primary physicians, gynecologists, and surgeons may not disclose such progress with the new subjects whom they evaluate.
This will leave behind the patient with a mastectomised flat chest, even though such a surgery as per modern studies is inferior to oncoplastic surgeries.
Breast cancer affects not only the body or physique but the mental trauma, anxiety, and agony is far beyond imagination. The first Question a lady with a diagnosis of breast cancer will ask to herself will be “Why God oh me? What in me has precipitated the cancer? Fate Karma?”
Then this will lead to denial, depression, anger, fear of recurrence, and finally “acceptance”. Mourning over the lost breast adds to trauma and external pads will never be incorporated into the body image.
Most of these women especially the young may have just entered into the professional career ladder, some may be just married, some unmarried, and others may have postponed pregnancy for a career, and getting a mutilating mastectomy further destroys the morale.
Hence Oncoplasty will be a boon considering the fact that breasts are a sign of beauty, symmetry and feminity. Offering a normal-looking, and feeling breast, on many occasions even preserving nipple and areola will help the lady to get adjusted to the further treatments with increased confidence.
A dedicated, and compassionate cancer surgeon, well trained in plastic and oncoplastic surgery is the pre-requisite to an excellent cosmetic outcome.

The emergence of a perforator artery-based flap, a local flap, has emerged as one of the versatile options to offer the best oncoplastic surgery for tumors localized in most of the quadrants of the breasts.
Morbidity to the “donor” area of the body like the back in the LD flap, lower belly in the TRAM flap, or gluteal region in the microvascular flap are well known. In perforator artery-based local flap that issue is avoided.
Common perforator arteries and flaps that are employed for such novel reconstruction procedures include, Lateral Intercostal Perforator Artery Flap (LICAP), Anterior Intercostal Perforator Artery Flap (AICAP), Combination of both (LICAP+AICAP), Middle Intercostal Perforator Artery Flap (MICAP), LICAP +AICAP combination could be used even for Mastectomy with Immediate Reconstructions (MIBR). Whereas, LICAP flap in general is the preferred flap for reconstruction of tumors located in the lateral, inferior, or central quadrants, after wide resections.
These novel concepts have paved a new way to address breast cancer management, in a different perspective to offer better confidence in the minds of women with breast cancer so that they could get solace at the earliest. It offers a better quality of life and confidence. Avoidance of morbidity to the donor area is definitely a boon because no scar marks of reconstructions(stigma) will be visible on the body.
Management of breast cancer has changed a lot over a period of time as technological improvement and understanding of genetics have become an integral part. Breast cancer is a lifestyle disease in more than 90% of the cases. Around 10% have a genetic predisposition. BRCA1, BRCA11, HER2, triple negativity, etc all have strong genetic links.
Obesity, lack of exercise, high fatty diet, red meat, lack of breastfeeding, late pregnancies, contraceptive pills, and fertility treatments with estrogens are all said to influence.
If one aims to have a 100% cure, early detection of cancer is a must. Breast self-examination (BSE) should be popularized which could pick up one cm-sized tumors. Ultrasound breasts and mammography could detect cancers in non-palpable stages. Another important fact is such mammographically detected tumors could be managed with wire localizations and scarless surgeries with no adjuvant treatments.
Personalized treatments, immunotherapy, and targeted treatments in addition to conventional treatments like chemotherapy or radiation after an oncoplastic surgery have paved the way to better cure rates.
Breast cancer is a curable disease in the majority of the early detected cases. Beauty could be restored. Why can’t we have a concerted effort to conquer the number one killer? Media has a large role to play in spreading the good news.

